The first time I was hospitalized for congestive heart failure, I was almost given twice the medication I was supposed to have at 3am. As soon as that was resolved, I grabbed the notebook that was beside the bed and started writing everything down. That was the beginning. Since that time, not quite every single place I go, I bring with me a notebook. In it, I have all of the phone numbers of my physicians, a copy of my medical history in outline and my current medications (usually 2 copies, so they can just keep one), and a list of time-tested questions in case I freeze up and forget to ask.
It helps me to remember that Brain Blank is entirely neurological at the most primal levels — it’s not that I’m not paying attention, or that I’m not smart enough, or even that my doctors are necessarily callous/over-hurried but that the brain copes with shock in incredibly unproductive ways (even small scale shock like being asked a question unexpectedly as in pop quizzes). There is a flood of cortisol and adrenaline so that you are ready to fight/flight without thinking, and that, by definition, turns off any part of your brain that would come up with good questions. It will also greatly minimize the likelihood of remembering the answers, so it truly truly is natural and normal to feel like medical appointments are a blur. Add to that sustained ‘shock’ like pain (either chronic or acute), stress of Life stuff, and the combination is pretty brutal in an exam room with the paper sheet and the dysfunctional medical gown. In sum: Having the notebook gives me something to do, which provides emotional distance, but mostly it means that I have something to refer back to when I come back from Paleo-Mind.
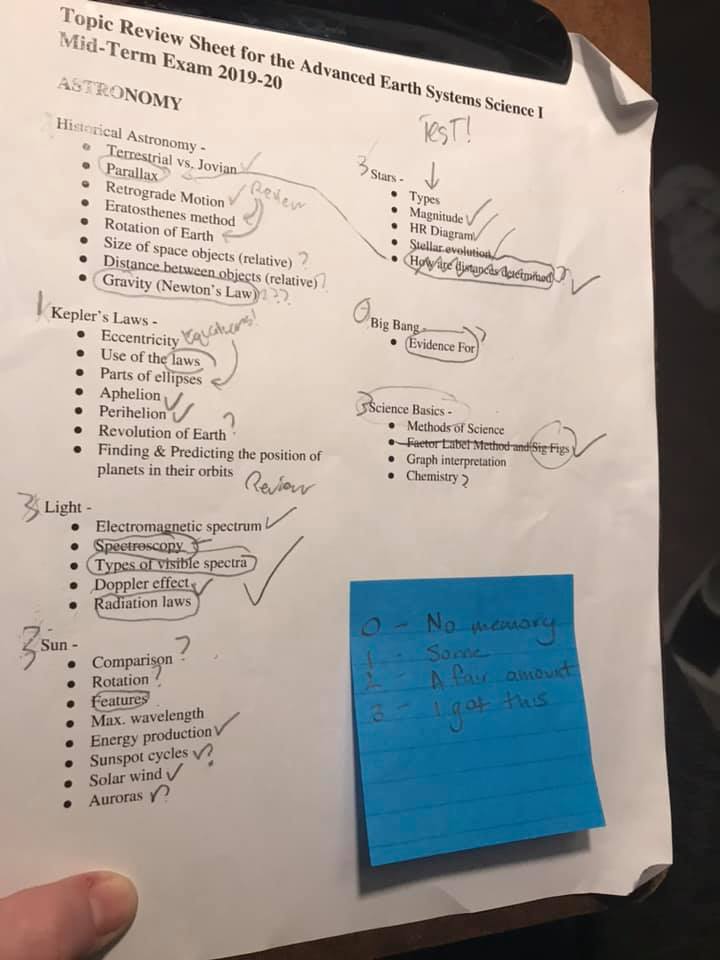
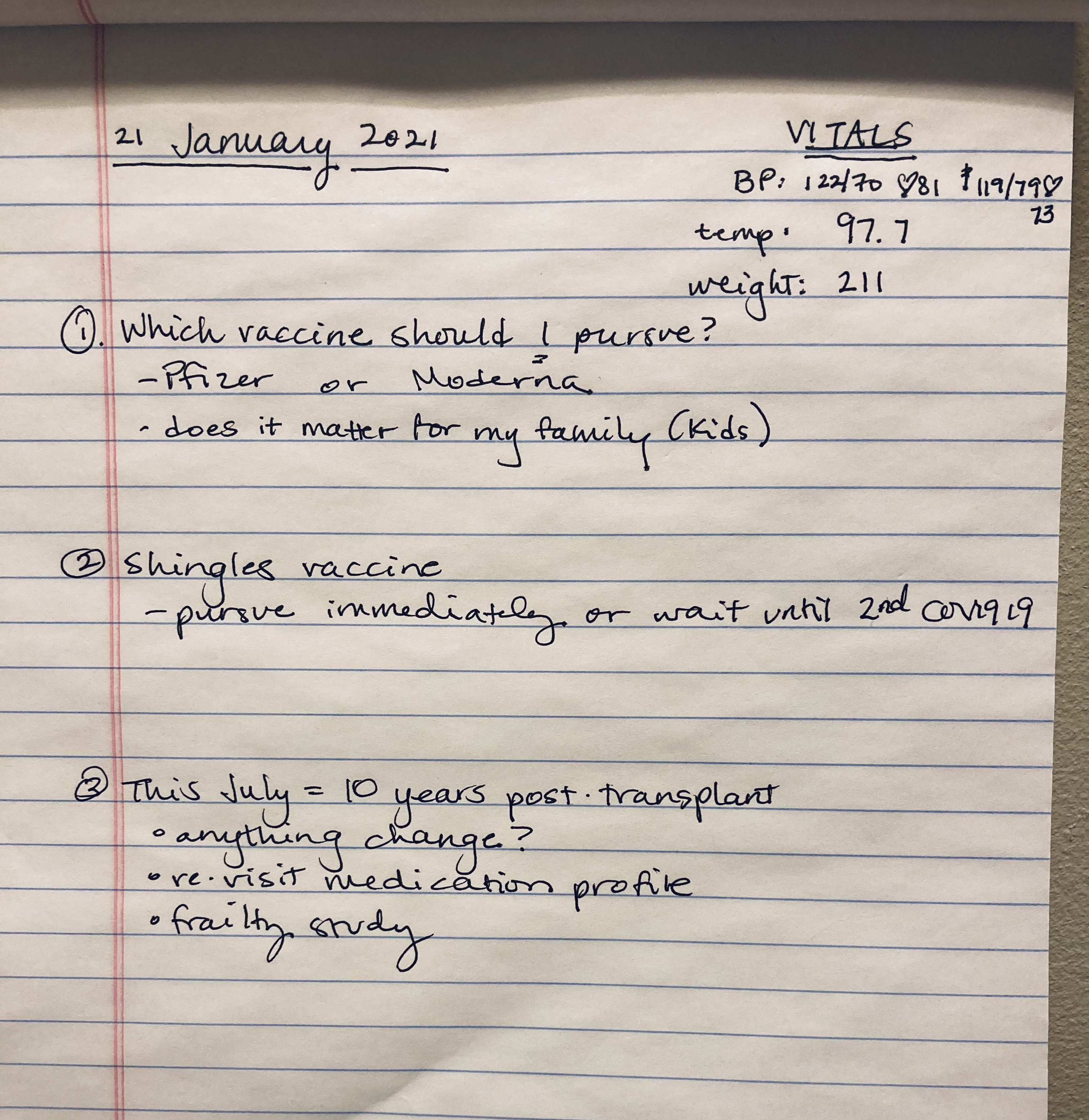
Before big appointments, I write out all of my questions and review them with my spouse (he often thinks of things I didn’t). I also rehearse and model this with my teens before their interactions with medical care teams.
The thing is, sometimes it is a challenge to even know what I should be asking about. I do not know the names for all of the parts of me. There are situations where I cannot see or ‘point to’ where the pain/concern is. I try to use a guide of presence (that is, “what are the circumstances when IT happens”) or absence (as in, “what are the circumstances where I WANT it to happen and it DOES NOT”). Even that can get twisted in a hurry: I have no basis of comparison from if other people experience the presence or absence of something the way that I do to know if what I am saying will contribute to meaningful problem-solving. The nature of my illness has included conversations I never imagined having (e.g., how often and how much I urinate), to conversations I desperately need to have but are taboo (such as how fatigue impacts libido in a partnership with someone who does not have chronic illness).
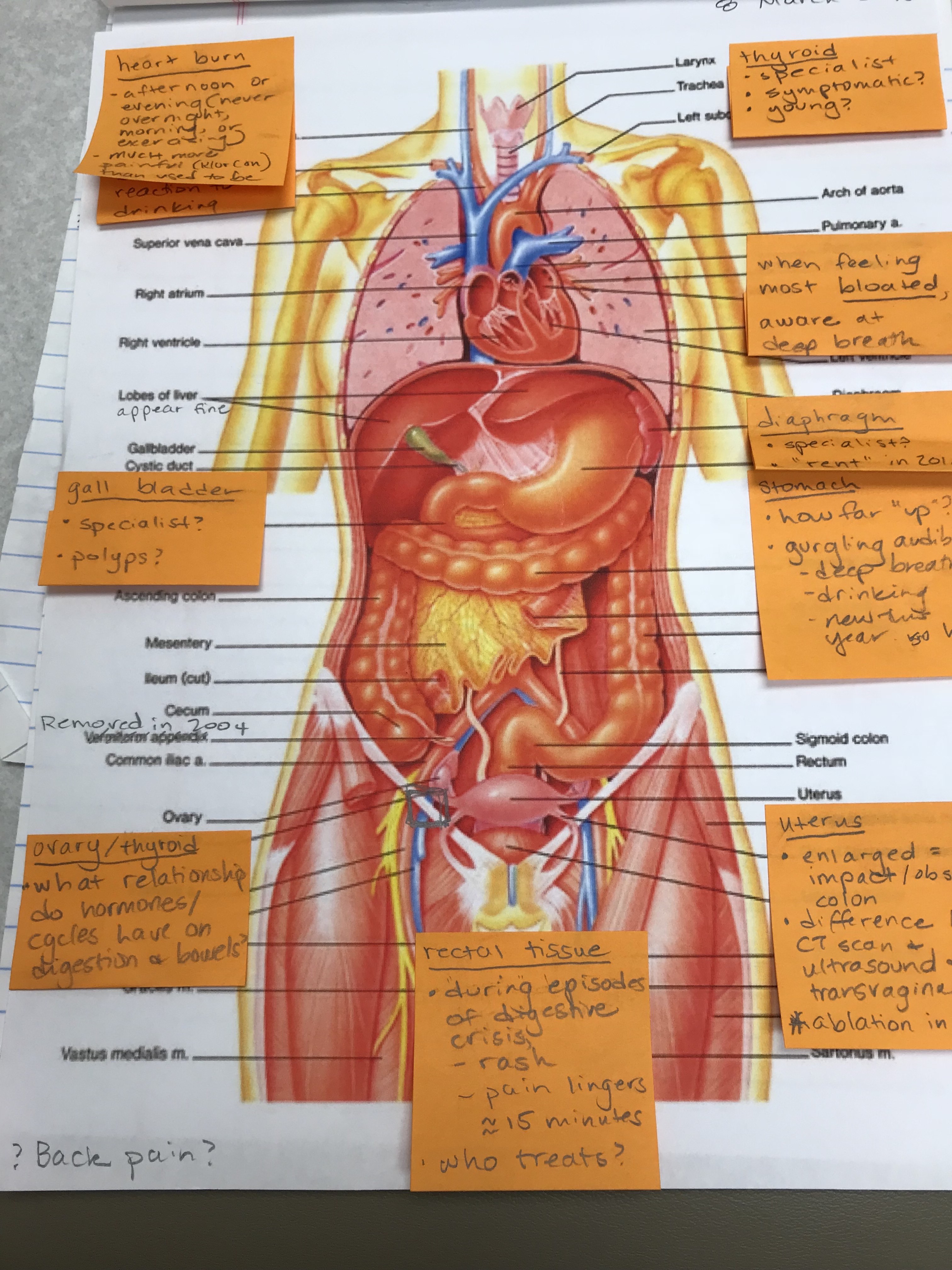
I try to come prepared to learn about my body and the care/keeping of it. I bring in materials to support conversation so that I know there is shared understanding of regions of the body and what to call them. I have asked “how can I be a better patient?” with the intention of advancing my understanding for future visits, or alerting the physician that I feel we are in an ineffective dynamic. I used to feel like a failure and a freak if the visit ended without resolution. If the specialist had no idea what I was talking about, it must be my fault. I absolutely do not believe that any more; however, that’s a journal for another day.
Before I leave almost all appointments I say the following: “Let me read back to you what I’ve written down and make sure I’ve got it right.” Because that’s my ritual, doctors who I see regularly know and anticipate this; and it’s a habit I’ve practiced so much, I really have not walked out of a room without at least those answers. I still get sprung with unexpected information or questions, which I hate like a pop quiz; but I have a specific plan and that has gotten me through. If during that review a doctor interrupts/corrects me, I write that down, and go through the whole thing again. My cynical side also feels like this has established me as a much more serious self-advocate than I might otherwise be, and since I am navigating across many, many specialists there have been a LOT of times where I could provide information (recommendations, dates, etc.), faster than they could look up in my file. It also means I have clear info to compare with second opinions.
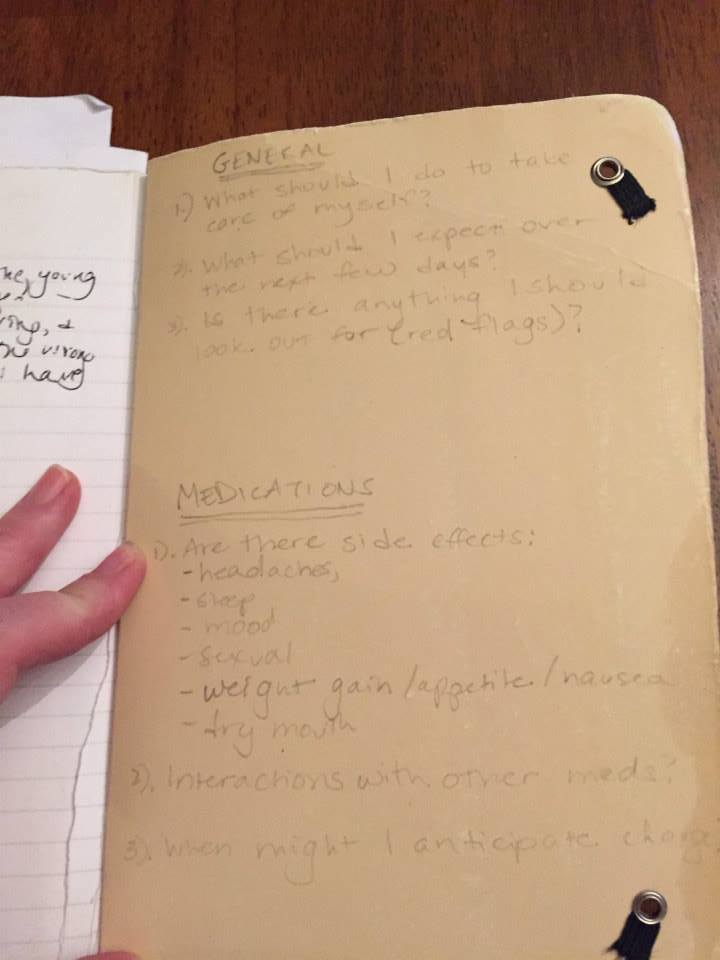
My “generic” questions are: GENERAL (1). What should I do to take care of myself? (2). What should I expect over the next few days? (3). Is there anything I should look out for (red flags)?
MEDICATIONS: (1). Tell me about the side effects: headaches, sleep, mood, sexual, weight gain/appetite/nausea, dry mouth? (2). Interactions with other medications (3). When might I anticipate change?
The answers to my General and Medications questions help re-orient me to being active in deciding IF I am going to pursue recommended next steps OR the conversation needs to continue (sometimes with another physician entirely). It is in my experience existentially critical to remember that “No, I’m not going to do that.” is mine to inhabit; it is true, and important. Knowing what my health status is and what my standards for quality of life are is critical to surviving and, ultimately, living -– those are not the same thing. Over the years I’ve come to rely on what I call the 4+1 questions as a structured way to think through recognizing and declaring when I am at this point.
I’m feeling tired, so that’s all I’m going to put for now.
End blip.