It’s a trick question on multiple levels: The list sentence format suggests that these are three distinct entities, and then parallel structure puts them all at odds from “something real”. What if they aren’t mutually exclusive?
What if they are all, each and overlapping, real?
I needed an entry framework for thinking about this, so I pulled together how the Mayo Clinic described the experience of Panic Attack, Complicated Grief, and Anxiety Disorders (General). Even at a glance, it was clear that Panic Attack and Anxiety Disorders have comparable lists. Complicated Grief has longer descriptions, and more of them. Next, I used color coding to cross reference — I used a red heading with Panic Attack, and any signs or symptoms that also appears with Complicated Grief (headed in blue) I made the text purple. Similarly, anything orange overlaps with Anxiety (headed in yellow). Those related signs or symptoms shared between Complicated Grief (blue) and Anxiety (yellow), I had the text written as green.
For a larger view of this thought experiment, here is a downloadable .pdf.
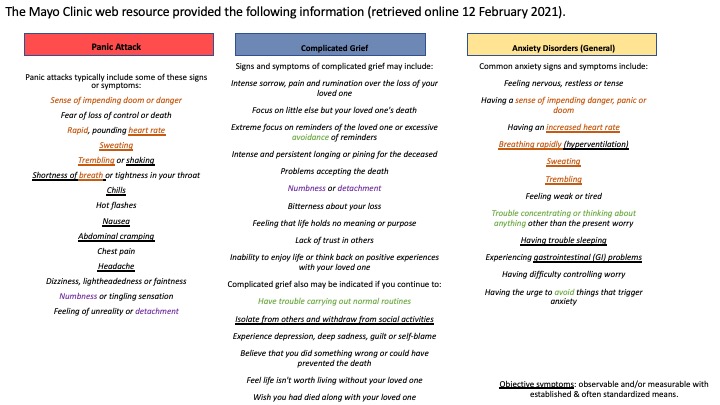
As a next step, I wanted to differentiate out subjective interpretations of experience, and bring awareness to “objective” elements (which are underlined). For my purpose I identified those as “observable and/or measurable by established and often standardized means.” For example, it surprised me some that the heart rate was not qualified. My own experiences with panic attacks and anxiety has found that sometimes I sense my heart is beating too fast or irregularly, but when checked on my cuff or during times I wore a harness monitor, there was nothing outside of the ordinary for a woman my age.
My distinctions are definitely arguable. “Numbness” has more than one meaning, one of which is an altered sensation of physical touch which can be measured with reliable, validated means ranging from minimally invasive sensitivity/awareness with a tongue depressor or Q-tip to more involved needle + electroshock measurements. I’m not certain that this is the meaning intended by how it is listed above. I think the more likely meaning refers to absence or dulling of emotional feeling, and that is a significantly more personalized impression.
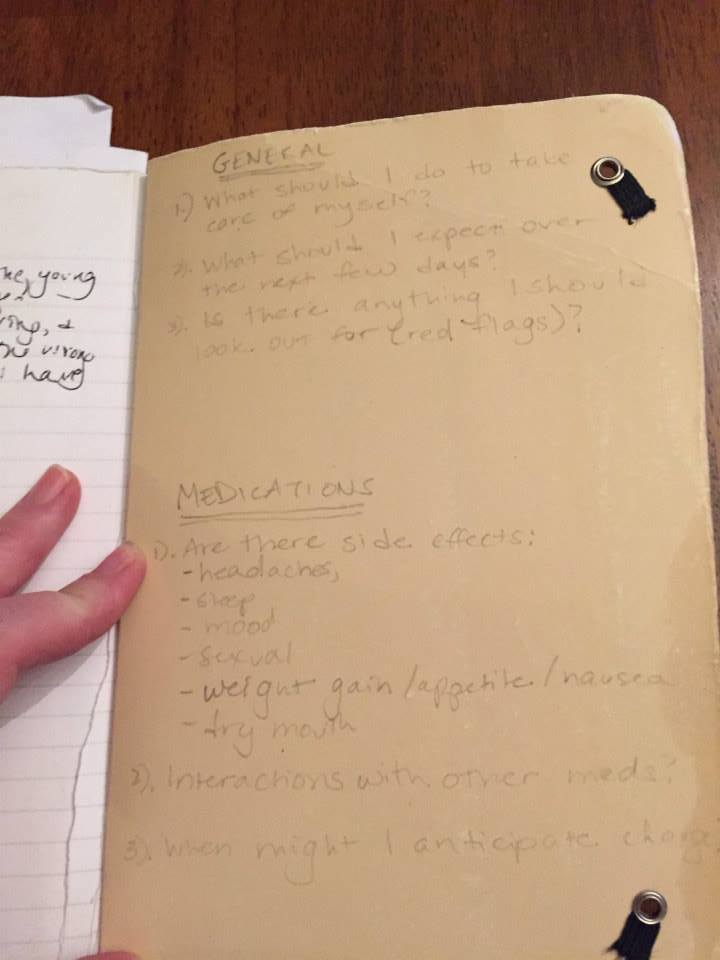
For a moment, I’m going to set aside how few objective symptoms are indicated under Complicated Grief, and that that is not what I originally set out to compare in this thought experiment (“Grief Ambush” was not listed at the Mayo Clinic website at the time of this writing). If a patient is a person like me with a long and diverse history of not-normal-for-a woman-my-age challenges + corresponding variety of patient portals, there is a calculation on my own of trying to figure out (a) what is happening, (b) how serious is it, and (c) who do I reach out to?

There are really only two reasons I would choose to go to an emergency room or outpatient clinic: 1) I know exactly what is going on, or 2) I am ready to die and do not want to do so at my home. When I am concerned I have a urinary tract infection (UTI) or question if I have broken a bone, an ER or outpatient clinic is fine. These kinds of problems are readily assessed and determined with clear paths of response. For other circumstances, it has consistently been my experience that we are a not a good fit for one another: they almost never have seen someone like me = a frustration and (liability) anxiety for them, and I end up with my belief that I am super weird beyond common medical practice confirmed again*.
*This statement contains many cognitive distortions which are not helpful. I see them and am staying with them for now.
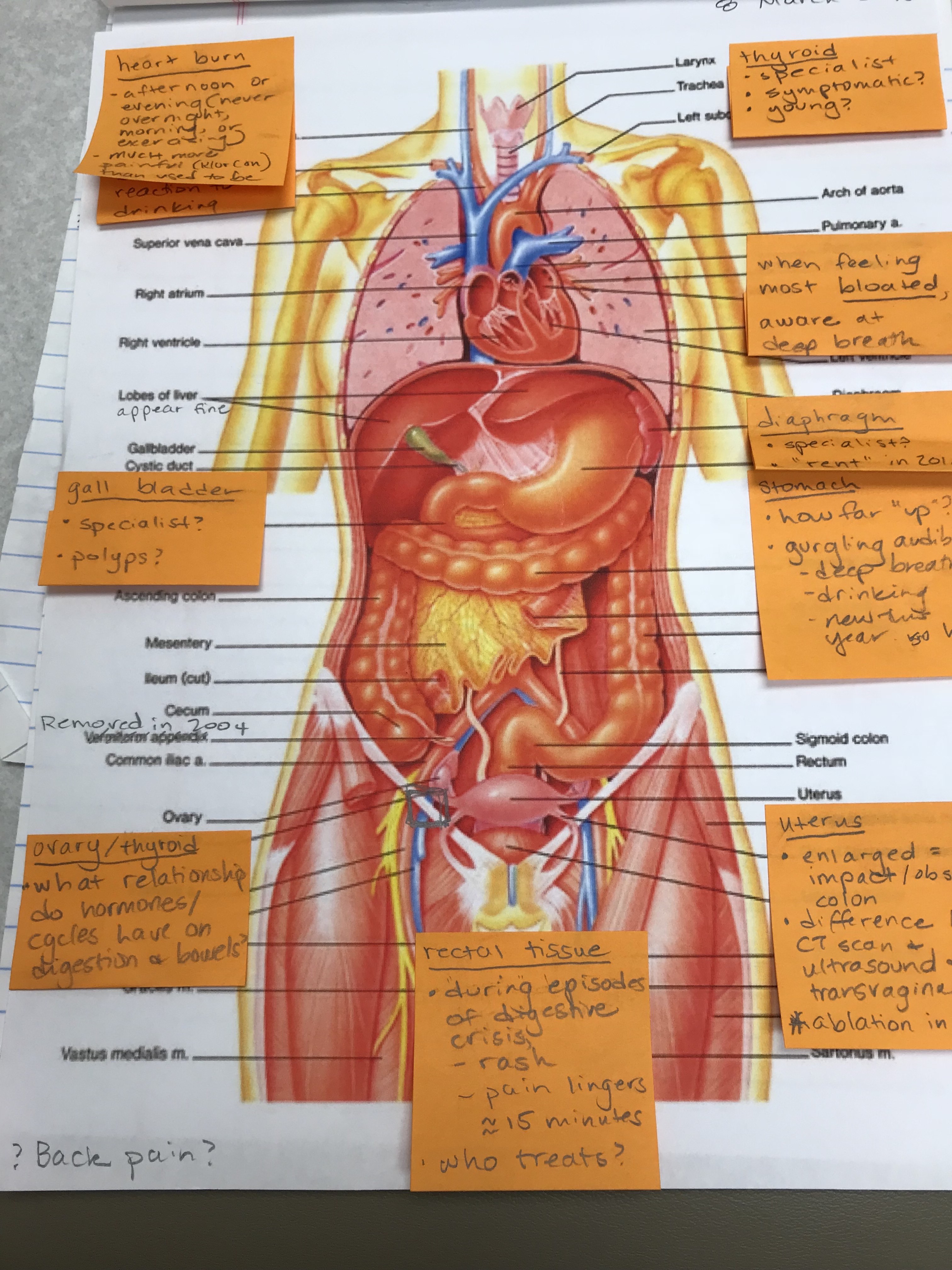
Heart rate, sweating, and trembling — overlapping between panic attacks and anxiety, or a problem with my hypertension (high blood pressure), OR maybe I exercised in a way that was unfamiliar to my ‘underconditioned’ body. Altered breathing is often a cause for alarm among some because I have a history of congestive heart failure. I’ve learned to understand additional elements such as whether I can lay completely flat comfortably (or feel like I am suffocating/gasping for air), and/or if I can continue holding a conversation while on a walk on an uneven surface. Aside: Knowing these are indicators of elevated concern with my heart history, if I experience them, I have to manage my emotional reaction so that I do not make the situation worse/more complicated. Upset stomach such as loss of appetite, nausea, or gastrointestinal (GI) distress? Could be a result of panic, anxiety — also grief, even though it is not mentioned — but I have been taking magnesium supplements for ten years now which carry known adverse effects of stomach problems, the potassium supplements sometimes come with abrupt heartburn, many of my other meds taste terrible (altering my interest and reception of other tastes), my gall bladder was removed in January of 2020 which impacts how I relate to food both in the moment and after, plus I am still available for all of the ‘regular’ ailments which turn the tummy such as a virus or food poisoning.
I confess: determining (a) what is REALLY happening, and (b) how serious is it REALLY, is complicated. I do not always know (c) who do I reach out to to figure it out, and that experience of not knowing has its own dimensions.
There’s that word again: complicated. At the top it was associated with grief, and I want to bring those two together and then bridge to the thing I was really aiming for (grief ambush). Complicated grief as a medical entity is associated with a timeline; accordingly, six months of a sustained presentation of the signs and symptoms listed will likely qualify. I am not in a position to say whether that’s a really long time to be living a life characterized by intense sorrow, pain and rumination or if that’s around when the majority of people begin to feel differently on average. There would likely of been a change in season, and time has a way of blurring edges.
Grief ambush though. There’s something acutely distinct about the overwhelm of memories, emotions, sensations, and thoughts that collapse from an unanticipated push of a lingering domino I didn’t know what still out there.

Simon and Garfunkel’s “Bridge Over Troubled Waters” was not just a song. It was the first song at my Dad’s funeral service, and quite possibly one of the songs at my Mom’s. I don’t remember that one as clearly (blurring of the edges). Why it was on my phone, in an album called “Unknown”, as a Track called 01, which was one of three Track 01’s is a mystery to me.
Cognitively, my mind went blank. Like an old-style t.v. that has been turned off: a burst, static, and quiet.
Physically, I no longer had a clear sensation of my body other than my hand holding the phone. I was a little dizzy as though my head were a helium balloon floating somewhere else. There was a heaviness in my upper chest.
And, I was not afraid. All of this was momentary. It had a familiarity. As the day wound away from this moment, I was physically depleted: low energy and appetite. Intellectually, I craved familiar and non-challenging content — I ended up re-watching a cooking show I’ve seen easily 5 times already.
It wasn’t until much later when I tried to problem solve how this song came to be on my phone in this way that I realized I held sorrow, too. It’s a beautiful song, and a sad memory. Now both of those each and overlapping, are real. Neither is “real” in a way that is objectively recognized with shared understanding and measurement.
That was when I realized it was the Loss Domino that tumbled into my thinking. That set a course for distinguishing panic, grief, and anxiety isn’t necessarily about whether they feel any different from one another. It’s about what thoughts they collide into, how I relate the then it bridges into my now, and who is in that moment with me.
End blip.