long before I saw it depicted for © 2007 Giske et al.
My earliest memories of being “not-well/whole” were both in 1982, when I was 8 years old. We were traveling in Mexico and at that time, water was problematic for persons not from the area. I remember clearly seeing the red tomato soup and orange soda before vomiting all over the restaurant table. I don’t have a visual memory of what happened next; only the sound of one of my parents chiding me for not going into the bathroom to throw-up, and the other parent chiding them that I probably would have if I’d known what was coming. Lesson: Whenever possible, be discreet with sick: others don’t want to see that. This was confirmed many times over the years by peers, educators, and faculty at every in-school vomit I ever witnessed.
Later that year, I took an abrupt fall on roller skates and ‘caught’ myself poorly with my left hand. There was a bracelet of bruise and I couldn’t move my hand, but it wasn’t swollen or at unusual angles. My parents and I went to the nearest Emergency Room, and I knew that they weren’t happy about the option because it did not have a reputation for quality of care. It was just the nearest one. Lesson: a person in pain may resort to the available response, not necessarily one they like or want.
I don’t remember anyone talking to me. I was wheeled into the x-ray room without my parents, and the technician kept positioning my broken wrist in ways that made me cry out. In retrospect, as an adult, I know he was doing that to get images of the breakage, but I think the only thing he said was, “stop screaming.” Lesson: Whenever possible, be discreet with pain: others shouldn’t have to deal with that. This was confirmed many times over the years by peers and family as soon as I joined the club of menstruators.
Thinking about it now, I didn’t have a pediatric dentist — I have no reason to believe that was a thing when I was a child. I saw one of parent’s dentists, who I have no recollection of ever saying anything to me other than to tell me I needed to brush more and floss. Lesson: Experts know when you aren’t following the rules of care, and will call you out if you lie.
I have vague memories of appointments with some kind of vision specialist for awhile. I have no idea, none whatsoever, what the goals were — watching rapidly presented photos of dominoes and told to call out the numbers, use a mirror to draw myself…I remember crying a lot. The man got upset with me for getting upset, but if there was a lesson in there somewhere I missed it entirely.
In grad school I saw someone for chronic migraines — my primary care physician, a headache specialist (is that a thing? I developed elaborate rating scales to note + characterize my daily pains and what, if any, patterns might be detected for catching when a headache was going to turn into a migraine so that medications that worked best in the first hour would be effective at all. Lesson: More data doesn’t necessarily lead to better answers and sometimes the answer medications offer isn’t much of one.
After grad school, I worked as a speech-language pathologist in a school district. Being a part of hundreds of meetings and forests of paperwork, I was the “expert” that was supposed to explain things — clear communication was my job. With all those kids, parents, educators, and other special area people, I developed and refined a sense of how to filter information, translate jargon, take notes, and ask probing questions. That inadvertently served me well when I became catastrophically ill. I’ve already written about my medical diary and questions, so my main point now is that I came into a process of learning how to navigate my body and interactions with others when unwell became explicit, intentional, and collaborative.
I wasn’t just showing up with my body of evidence for someone else to tell me what had happened, was happening, might happen next. My being chronically ill pretty well exactly paired with my parenting, and over time I began thinking more and more about explicitly, on-purpose teaching my kids along with their other parent and medical teams they encountered.
For example, when I read:
- Dr. Atul Gawande’s books, Being Mortal, Better and
- Dr. Arthur W. Frank’s, The Wounded Storyteller: Body, Illness and Ethics (2nd Edition)
we talked about them over dinners, read excerpts together, referenced these ideas when current events featured health or medicine, and practiced increasing self-advocacy with respect to their own medical-emotional health.
Sometimes it was an overlap between my health and this goal. As in, it was during the time when a new blood pressure medication was making my vision blurry that I realized I shouldn’t be the one reading over the counter medication labels for them: as teens, it was appropriate that we should transition to supporting their decision-making in listening to their body and taking steps, knowing about dosages and timing schedules.
It wasn’t until more recently when a friend shared with me the 2007 article, A Personal Experience of Working with Classical Grounded Theory: From Beginner to Experienced Grounded Theorist by Tove Giske and Barbara Artinian that I came to understand what this process was:

The only thing I might add to Figure 4, Model 13 from my personal experience is
- a loop — that this is a repeating cycle, not finished in the way “conclusion” often implies, and
- some vehicle for storytelling: sharing lessons learned with others, hearing and learning with theirs.
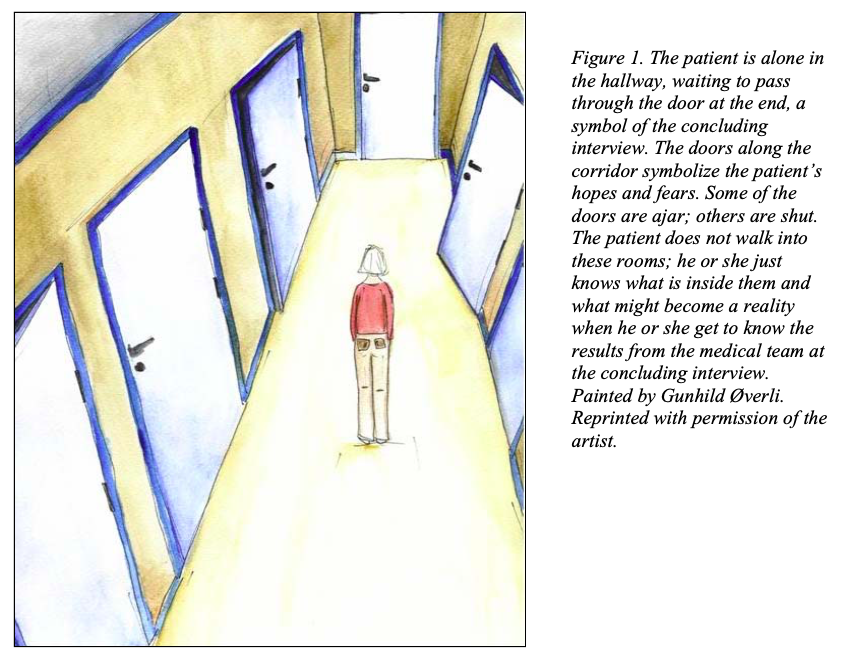
For me, the sharing component is similar to “Balancing between hope and despair”: it is a filter or prism that influences all of the other aspects of preparative waiting. The figure in the hall, the patient, in so many respects may be alone. However, there are resources to be found within their framework of preparative waiting:
- to have heard about the seeking and giving of information in medical-emotional health experiences of others (e.g., this is what happened with me),
- to know what kinds of clues there might be and perspectives of interpreting (that is, how I saw, heard, felt, came to understandings, etc., along the way),
- community references around cultures, spiritual and philosophical practices in handling the existential threat within “why is this happening to me” and “what does it mean?”
- and giving and receiving among one another meaningful support and tools for establishing spaces of calm within the inherent chaos and uncertainty whether or not respite is sought. Rest from thinking, wondering, imagining, dreading, worrying, grieving; recuperation from all the moving around that comes with being acted upon (even in the service of diagnosis).
Towards that end, I find myself at this end: it is time I rest my mind from this.
Conclusion of blip.